
- Lower extremity compartments fasciotomy update#
- Lower extremity compartments fasciotomy full#
- Lower extremity compartments fasciotomy free#
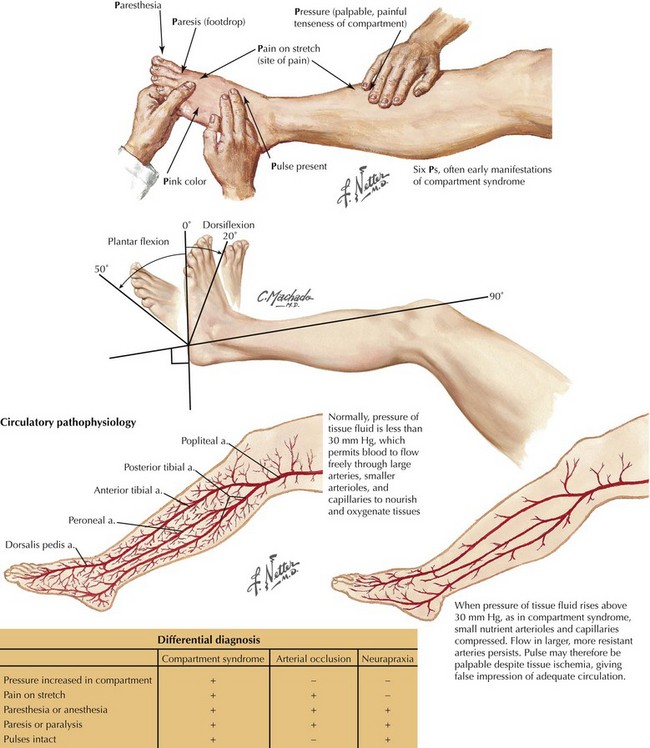
Decompressive fasciotomy for acute compartment syndrome of the leg. Owen C, Cavalcanti A, Molina V, Honore C. Lower extremity fasciotomy: indications and technique. Compartment syndrome of the lower extremity. Gluteal compartment syndrome with sciatic nerve palsy caused by traumatic rupture of the inferior gluteal artery: a successful surgical treatment. The pressure threshold for decompression. Compartment monitoring in tibial fractures. Compartment pressure in association with closed tibial fractures: the relationship between tissue pressure, compartment, and the distance from the site of the fracture. Heckman MM, Whitesides TE Jr, Grewe SR, Rooks MD. Accuracy in the measurement of compartment pressures: a comparison of three commonly used devices. Compartment syndrome: an orthopedic emergency. Serum creatinine kinase levels are associated with extremity compartment syndrome. Valdez C, Schroeder E, Amdur R, Pasual J, Sarani B. The pathophysiology, diagnosis and current management of acute compartment syndrome. Intracompartmental pressure measurements in the normal forearm. Seiler JG III, Womack S, De L’Aune WR, Whitesides TE, Hutton WC.
Lower extremity compartments fasciotomy update#
Acute compartment syndrome: update on diagnosis and treatment. Incidence and predictors for the need for fasciotomy after extremity trauma: a 10 year review in a mature level I trauma center. 2017 217:131–6.īranco BC, Inaba K, Barmparas G, Schnüriger B, Lustenberger T, Talving P, et al. Extremity compartment syndrome following blunt trauma: a level I trauma center’s 5-year experience. Zuchelli D, Divaris N, McCormac JE, Huang EC, Chaudhary ND, Vosswinkel JA, et al. Acute compartment syndrome: who is at risk. Review: acute compartment syndrome of the foot.
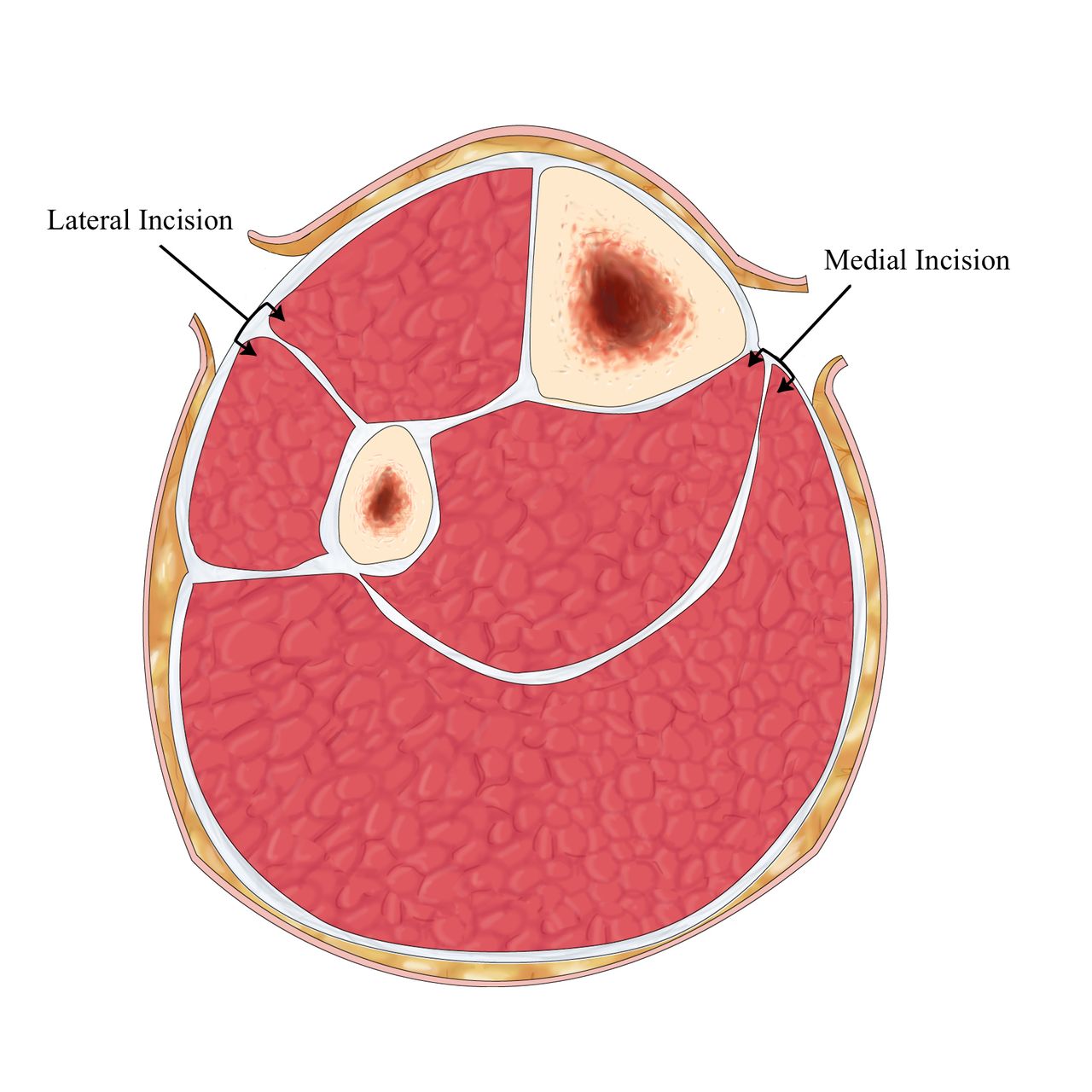
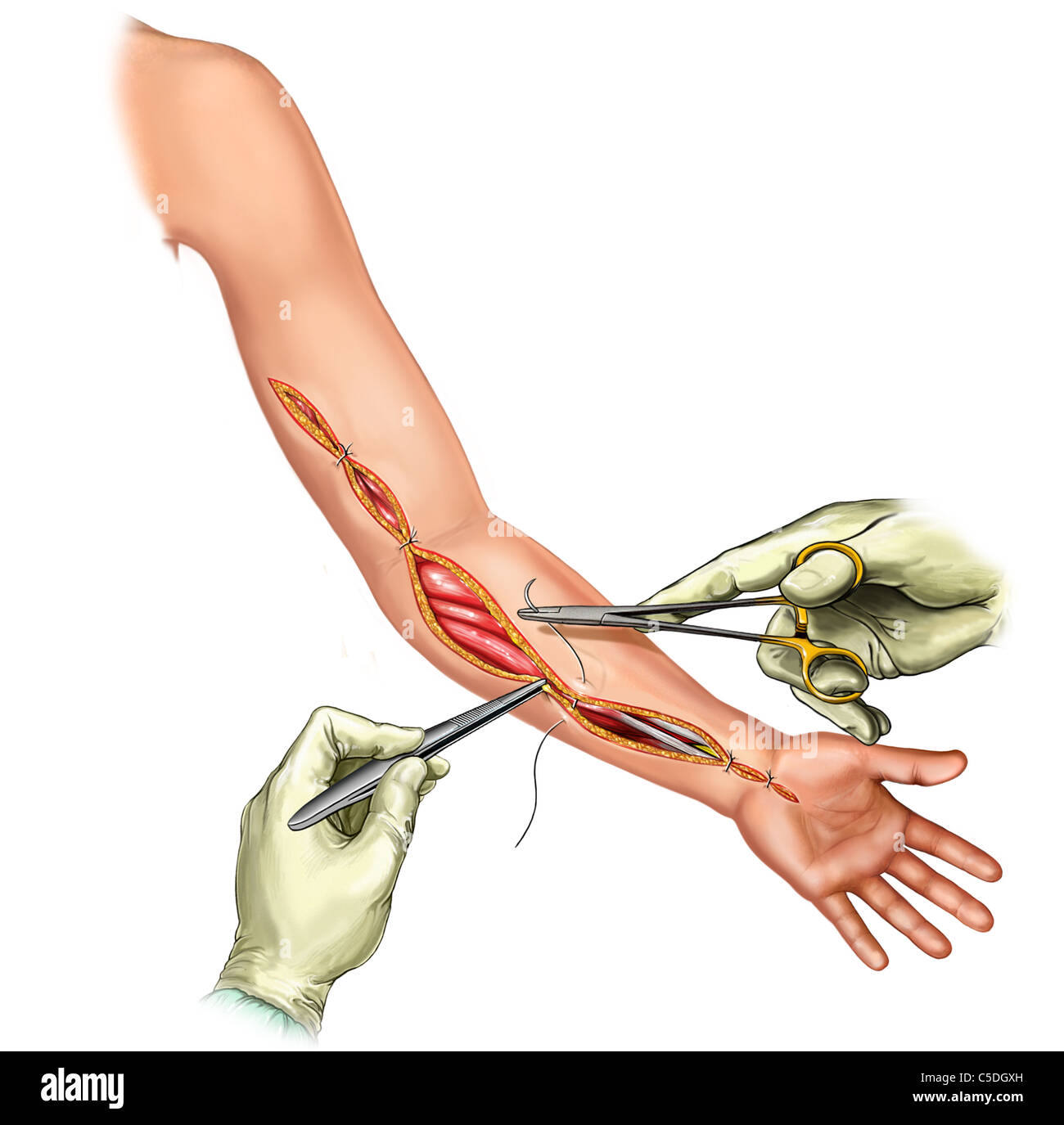
Landmarks used to accurately position incisions will also be described. This chapter will describe location and content of the compartments.
Lower extremity compartments fasciotomy full#
Surgeons need to be familiar with the location of compartments in the extremity in order assure full decompression during fasciotomy. In these cases, laboratory studies and compartment pressure measurements added to clinical findings improve early recognition. Clinical symptoms though present may be masked by other injuries, medications, peripheral blocks, or mental status changes. Patients with patterns of injuries likely to result in raised tissue pressures are at risk of developing compartment syndrome. Identifying patients that require fasciotomy can be a challenge. Injury to the limb is a common predisposing factor among patients requiring fasciotomy making it an important skill for surgeons caring for trauma patients to do competently. When fasciotomy to treat acute compartment syndrome (ACS) is delayed or done incorrectly, permanent disability, limb loss, organ failure, or even death is possible. Begin with strides and slow jogging forward and backwards, side to side and diagonals.Extremity fasciotomy is a procedure that may save a life or limb when performed correctly.Progressive strengthening exercises using higher stability and neuromuscular control with increased loads and speeds, along with combined movement patterns begin with low velocity, single plane activities and progress to multi-plane high velocity.Avoid pain with any exertional activity.
Lower extremity compartments fasciotomy free#


 0 kommentar(er)
0 kommentar(er)
